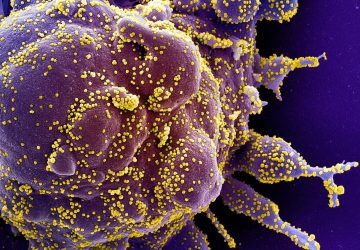
In a pandemic, quick at-home testing is essential not just for isolating cases but also for compiling big picture data. When COVID-19 struck, however, all the common rapid testing formats were laborious to use and tough for non-specialists to interpret. So Professor Sam Sia, an expert in point-of-care diagnostics and therapeutics, decided to pivot his research to address the crisis. Sia’s lab has spent the past few months developing simple tools that yield nearly instant results—a prime example of how his group designs miniature medical devices for major impact.
How would you sum up the big idea animating your research?
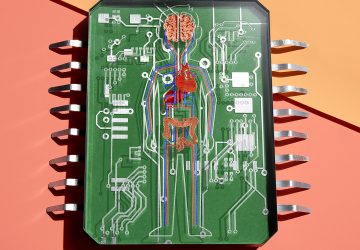
Miniaturizing devices will transform medicine the way microelectronics has transformed communication. That could mean anything from developing quick and inexpensive blood tests that can be deployed anywhere, anytime to designing tiny, implantable tech for continuously monitoring and treating patients.
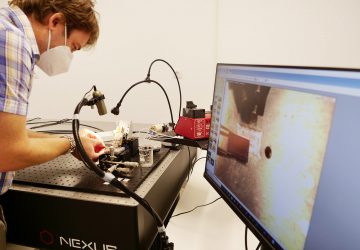
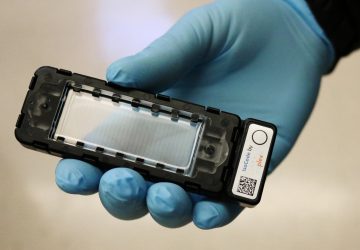
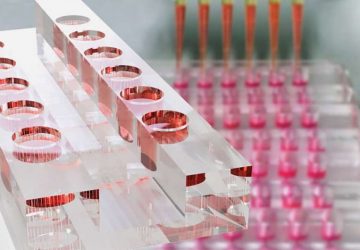
On the testing front, my group, alongside a startup company Rover Diagnostics, has been working hard on a new rapid COVID-19 test based on reverse transcription polymerase chain reaction (RT-PCR). We are now participating in the National Institutes of Health “Rapid Acceleration of Diagnostics” initiative to refine and validate the system.
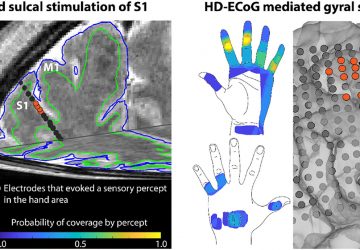
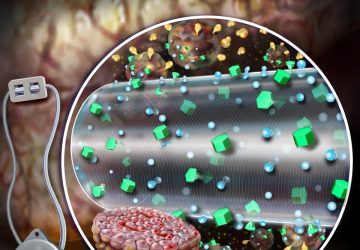
In terms of implantable tech, we focus on devising miniaturized devices that are biocompatible and controlled wirelessly in the body to monitor people’s health and treat various conditions.
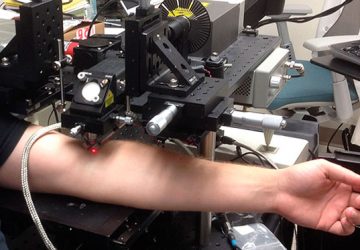
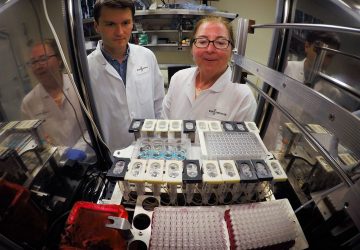
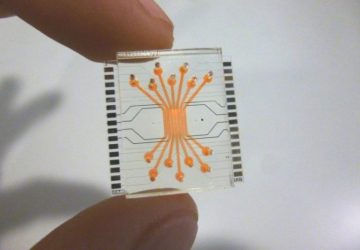
Your group has had a lot of success miniaturizing devices by using microfluidics, which manipulates minute amounts of liquids to conduct precise experiments. This field has only been around since about the 1990s. What most captures your imagination about the promise of this rapidly emerging technology?
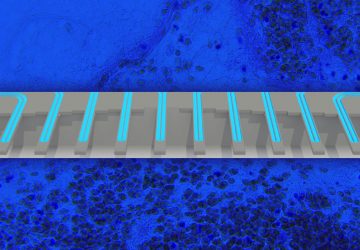
Medicine in the past has been approached biochemically, but through microfluidics—which are cheap to build and easy to transport—there’s a huge opportunity for devices to dramatically improve diagnostics and therapeutics, especially in low-resource field settings around the world. Take the Lyme disease test we developed earlier this year. This test uses a microfluidic chip to create the first point-of-care device that can diagnose Lyme in under 15 minutes.
These are the kinds of tools we want to put into the hands of practitioners. In my lab, we work closely with clinical doctors and combine insights from biology, chemistry, medicine, data science, and consumer electronics to design low-cost, integrated devices that are field ready.
What are some things happening in your lab right now you’re particularly excited about?
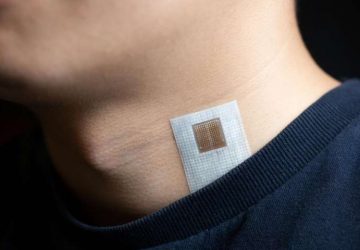
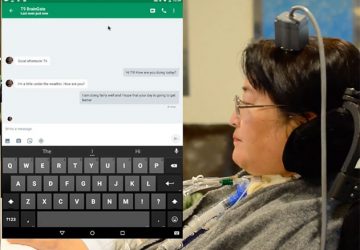
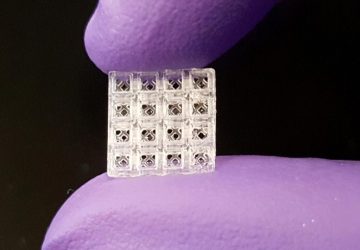
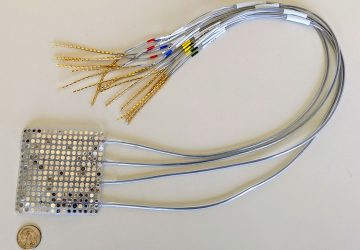
In the realm of diagnostics, the combination of wearable devices and data analytics is moving from theory to practice; I’m excited that we’re situated right at the intersection of this impending transformation. There’s two projects in particular that I think are good illustrations of our approach here. In relation to COVID-19, we’ve been concentrating on making rapid test formats easier to use at home in part through a mobile app leveraging computer vision and machine learning to interpret test images and provide individualized guidance. We’re also collaborating with Professor Ken Shepard on a DARPA-funded project to develop an “active” bandage using implanted components and machine learning to help the body heal its wounds faster.

source: www.bme.columbia.edu