The Dec. 19 FDA approval of Spark Therapeutics’ gene therapy to treat a rare form of inherited blindness has energized ongoing efforts to find new ways of repairing faulty genes or cells in multiple diseases—including diabetes. Today scientists at the University of Pittsburgh School of Medicine announced significant progress in their efforts to use gene therapy to reverse diabetes.
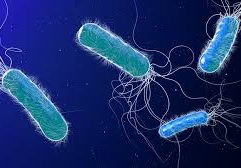
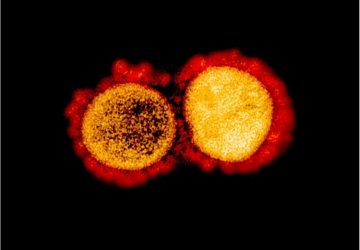
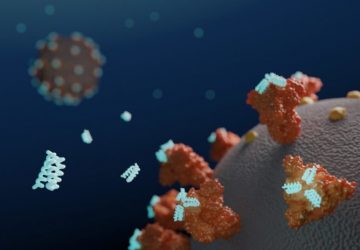
Type 1 diabetes occurs when the immune system mistakenly destroys insulin-producing beta cells in the pancreas. In mouse models of Type 1 diabetes, the researchers demonstrated a gene therapy approach that transforms alpha cells in the pancreas into fully functioning beta cells. They described the technique in the journal Cell Stem Cell.
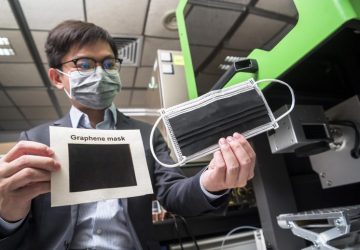
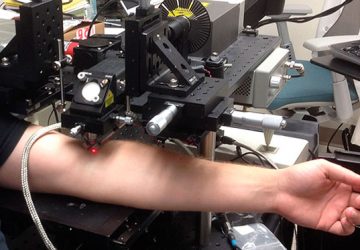
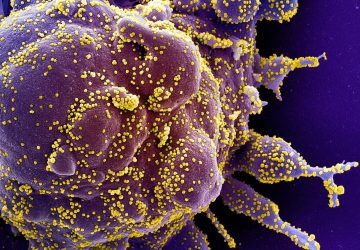
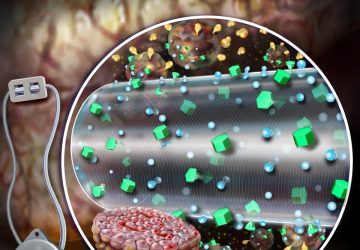
The team used an adeno-associated viral (AAV) vector—the same technology that’s at the heart of Spark’s gene therapy—to deliver two proteins, Pdx1 and MafA, into the pancreas. These proteins “reprogrammed” alpha cells into insulin-producing cells, according to a press release from the university. The mice maintained normal blood glucose levels for about four months.
“This study is essentially the first description of a clinically translatable, simple single intervention in autoimmune diabetes that leads to normal blood sugars,” said lead author George Gittes in the statement. He added that the treatment did not cause the immune system to become depressed—a major risk of treatments designed to correct autoimmune disorders.
RELATED: Harnessing immunotherapy to reverse Type 1 diabetes
One potential advantage of transforming alpha cells into beta cells is that alpha cells are distinct enough that the immune system is unlikely to mistake them for beta cells and attack them. The researchers compared gene expression patterns between normal beta cells and the alpha cells that they transformed into insulin producers and determined they had achieved “nearly complete cellular reprogramming,” according to the statement.
Many of the new approaches being tried in diabetes center around tricking the immune system into behaving properly. For example, scientists at Cardiff University School of Medicine in the U.K. are working on a technique that involves using a proinsulin peptide to prevent destructive immune cells from attacking beta cells. And researchers at Massachusetts General Hospital are testing the tuberculosis vaccine bacillus Calmette-Guérin (BCG), which they discovered has the ability to restore regulatory T cells (Tregs)—immune cells that halt the destruction of beta cells. And in November, a team at Boston Children’s Hospital published evidence that boosting the immune checkpoint protein PD-L1 may prevent the destruction of insulin-producing cells.
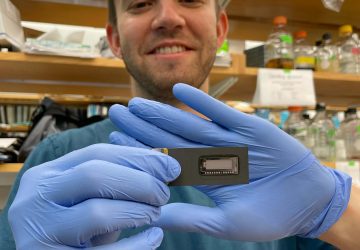
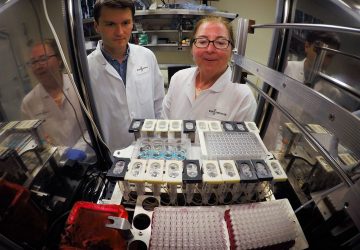
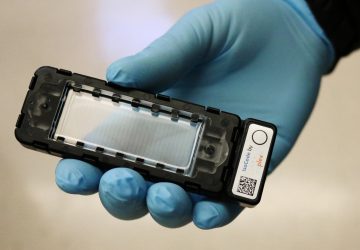
Gittes and his colleagues at the University of Pittsburgh are concerned that the mice they treated with gene therapy eventually returned to a diabetic state, though they say more research is needed to determine how the duration of response would translate to people. They are currently testing the technique in primates and plan to seek FDA approval to run clinical trials in people with either Type 1 or Type 2 diabetes.
source: www.fiercebiotech.com