Study shines light on how to build better bacteriophage therapies
Researchers have discovered that a subset of bacteriophages, dubbed “superspreaders,” potentially play a major role in transmitting antimicrobial resistance. The research, described in a study published this week in the journal mBio, provides an answer to a long-standing biological question and may help scientists better select specific bacteriophages for therapeutic use.
“Our work suggests that phage superspreaders may help drive bacterial evolution in natural environments but are not suitable for use in medicine,” said lead study author Eric Keen, a graduate student at Washington University in St. Louis, Missouri, who conducted the project at the University of Miami in Coral Gables, Florida and at the National Cancer Institute (NCI), in Bethesda, Maryland. “We think our findings are something that clinicians and researchers should be aware of because different phages seem to disseminate antibiotic resistance genes at different rates. Obviously, we don’t want to be designing therapies using phages which are efficient at spreading antibiotic resistance genes across a bacterial community.”
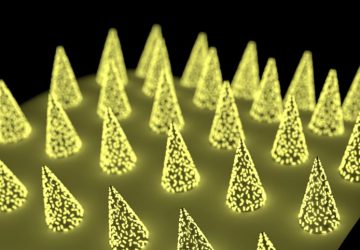
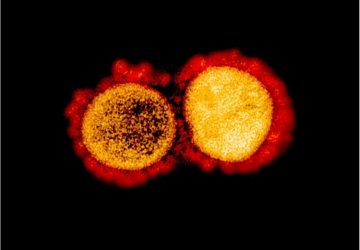
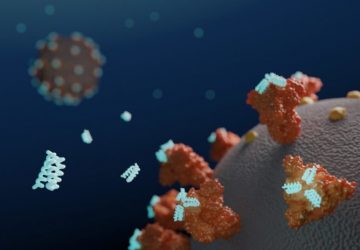
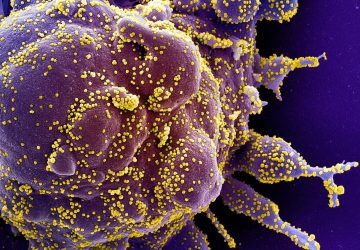
Bacteriophages, viruses that infect bacteria, are the planet’s most numerous microorganisms. They kill vast numbers of bacteria in natural environments, and in a few countries such as Georgia and Poland, bacteriophages have been used to treat bacterial infections. With the rise of the antimicrobial resistance, there has been renewed interest into using bacteriophage therapy in the United States and Europe.
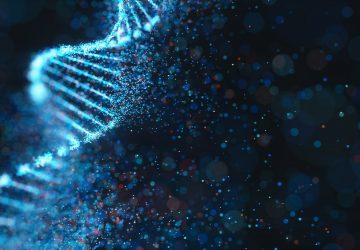
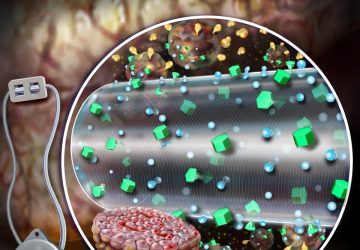
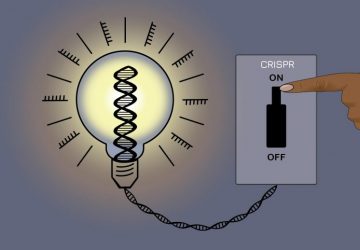
While scientists have known that many bacteria carry plasmids, extrachromosomal DNA elements that frequently encode antibiotic resistance, nobody had previously studied what happens to these plasmids when an invading bacteriophage blows apart a bacterial cell. “It has not been known whether plasmids are destroyed during phage infection or released intact upon phage lysis, whereupon their encoded resistance could be acquired by other bacteria,” said Mr. Keen.
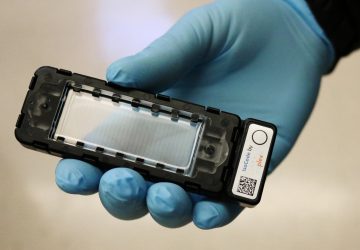
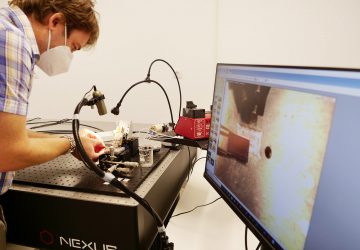
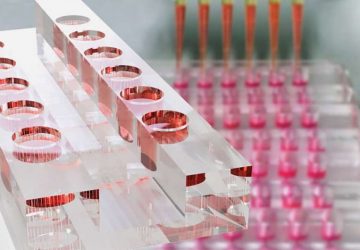
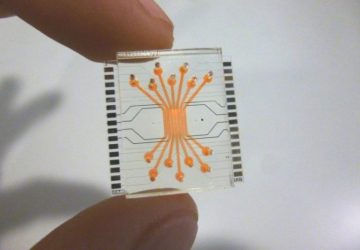
To solve this knowledge gap, researchers from the University of Miami and the NCI assembled a library of environmental phage isolates from environmental samples, including soil samples from Maryland and canal water in Florida. They infected Escherichia coli strains resistant to the antibiotic ampicillin with 20 different phage isolates and then measured the amount of plasmid DNA released intact upon phage lysis.
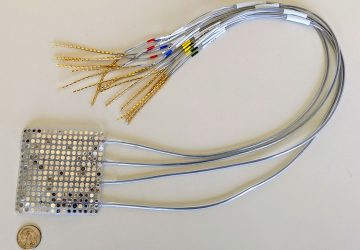
The researchers found that two of the 20 bacteriophages promoted plasmid transfer 50-fold in excess of that seen with the other 18 phages and that these two phages were able to efficiently release several different plasmids, each carrying a different antibiotic resistance gene. The researchers called these two bacteriophages SUSP1 and SUSP2, short for superspreader. “We coined that name because we thought what we were seeing was evocative of a phenomenon in epidemiology in which you have an outsized transmission by a relatively small percentage of the overall population,” said Mr. Keen.
Additional experiments demonstrated that SUSP2 encouraged the transfer of antibiotic resistance to communities of soil bacteria from Maryland and Wyoming. Adding SUSP2 to co-cultures of kanamycin-resistant E. coli and kanamycin-sensitive Bacillus bacteria resulted in roughly 1,000-fold more kanamycin-resistant Bacillus bacteria than arose in phage-free controls, suggesting that this phage might be able transfer antibiotic resistance genes to bacteria besides E. coli and under more natural conditions.
The researchers characterized the biology of the two phages using electron microscopy and genome sequencing. “Based on our work with a number of different mutants of well-characterized phages, we hypothesize that the reason these two phages are special is because they lack hydrolytic endonucleases that other phages use to chop up DNA very efficiently during infection,” said Mr. Keen. “We think that superspreaders lack these enzymes, and as a result DNA survives their infection basically intact.”
He said researchers should steer clear of the “superspreaders” when designing bacteriophage therapies, noting that the majority of phages tested were far less efficient at promoting antibiotic resistance transfer. Future research directions include a more comprehensive assessment of the specific underlying mechanisms of the superspreaders and an evaluation of the prevalence of the phenomenon in natural environments, including in the human body.
source : www.sciencedaily.com