Is your diet working? A new ingestible gas sensor may be able to tell.
An Australian team has developed the first gas-diagnosing intestinal pill ever to be tested in people. As the researchers report today in the journal Nature Electronics, this ‘smart’ capsule reliably measured levels of oxygen, hydrogen, and carbon dioxide as it journeyed through the innards of six healthy volunteers, revealing the impact of dietary fiber intake on microbial activity in the small intestines and colon.
Not only might this electronic pill one day shape custom diets for optimal gut health; it could also help doctors distinguish between the early signs of different GI disorders, such as malabsorption syndrome, Crohn’s disease, colitis, irritable bowel syndrome, and even colon cancer.
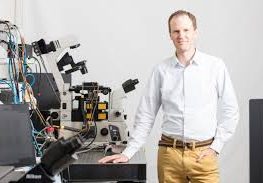
“At the moment, we have no tool to differentiate between these different things,” says Kourosh Kalantar-zadeh, an electronic engineer at RMIT University in Melbourne, Australia, who led the research. A colonoscopy can only reveal inflammatory lesions or cancerous polyps that are visible with a camera—and by that point, people have often suffered with gut discomfort and without a diagnosis for years.
“That’s too late,” says Kalantar-zadeh, who envisions people popping a swallowable sensor once or twice a year to detect disease early on. “If gas profiles around the norm change,” he explains, “then we’d know we have a problem with the gut.”
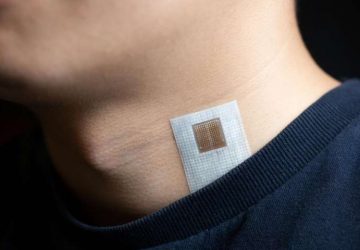
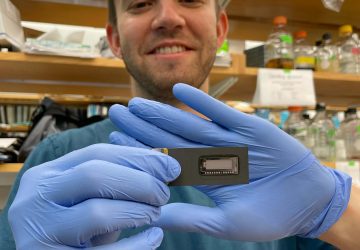
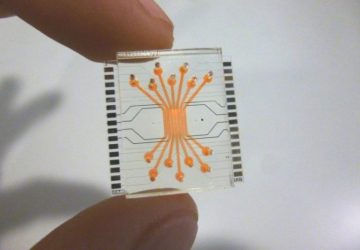
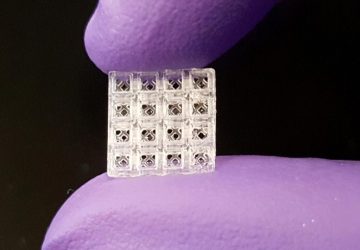
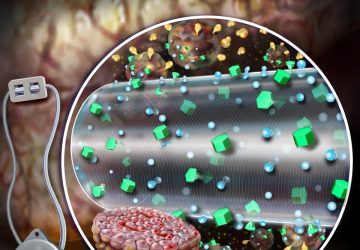
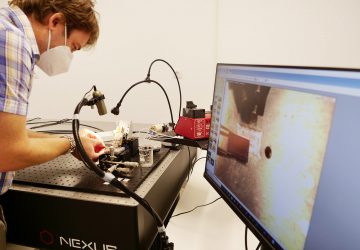
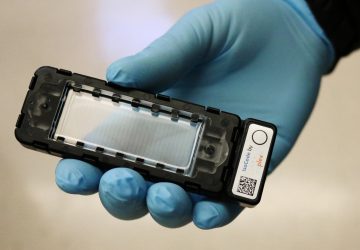
On its surface, the gas capsule looks like an over-the-counter supplement you’d buy at any GNC or Vitamin Shoppe. But within its inch-long polyethylene shell are two gas sensors, a temperature sensor, a microcontroller, a radio-frequency transmitter, and button-sized silver-oxide batteries. The gas sensors are sealed within a special membrane that allows gas in but keeps out stomach acid and digestive juices.
The system is an upgraded version of one that the Australian team previously tested in pigs. It determines gas profiles in the gut by modulating the heating elements of the sensors. Since oxygen, hydrogen, and carbon dioxide all conduct heat to different degrees, the sensors can accurately determine the levels of these gases by taking measurements at multiple temperature points.
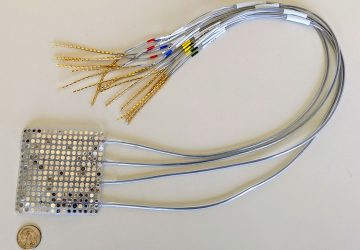
An algorithm reads the information coming off the sensors and relays the signal in real-time to a small receiver that has a range of up to 100 feet and can be carried in a pocket or left on the nightstand when someone is home. The receiver in turn transmits the data via Bluetooth to a cell phone, which can post the data online for easy monitoring by users and doctors.
Digital pills on the market today can already gauge things like pH and pressure inside the intestines. Some can also relay pictures of the esophageal and stomach lining. Plus, late last year the U.S. Food and Drug Administration approved the first sensor-enabled medicine, a version of an antipsychotic drug that’s embedded with sensors to tell doctors whether, and when, patients with schizophrenia take their pills.
But Kalantar-zadeh’s ingestible capsule, if it stands up to greater clinical scrutiny, would be the first to provide information about the chemical composition of the gut.
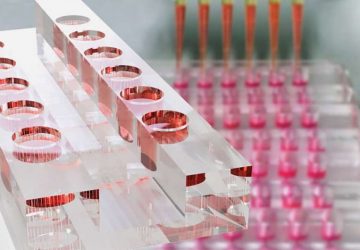
For the pilot trial, Kalantar-zadeh teamed up with nutritionists and gastroenterologists from Monash University to test the capsules in two men and three women, all of healthy weight, who were fed either a low- or high-fiber vegan diet for two days. (Another man also received both menus spaced two weeks apart.) The high-fiber diet consisted of things like nuts, broad beans, pears, figs, and whole-grain bread, while the low-fiber fare included tomatoes, cucumbers, lettuce, watermelon, and white bread.
The levels of oxygen-containing molecules picked up by the sensors told the researchers where the pill was situated within the gut. That’s because oxygen concentrations are known to drop over the course of the 30-foot long digestive tract, from the oxygen-rich stomach to the nearly anaerobic colon. Kalantar-zadeh and his colleagues confirmed the accuracy of this positional extrapolation by imaging the pills directly with ultrasound.
They then quantified the extent to which bacteria in the various intestinal compartments were actively breaking down food and liberating nutrients for their hosts by reading levels of hydrogen, a natural byproduct of microbial fermentation. (To some extent, carbon dioxide profiles offered a similar readout, although this proved less informative because CO2 is produced both by bacteria and our own cells.)
By analyzing all the gases concurrently, they could discern, for instance, why one person in the trial became constipated after eating the low-fiber diet: Oxygen levels placed the pill in his colon and the lack of hydrogen showed that this man’s gut bugs were mostly dormant. Only after he ate some fibrous food again did his colonic hydrogen levels spike—which explains why his bowel movements returned as well.
“They have demonstrated a fully integrated platform,” says Sameer Sonkusale, an electrical engineer and materials scientist at Tufts University, who was not involved in the study. “It’s truly an engineering effort.”
Clinicians who specialize in studying the impact of diet on gut microbes agree. “Overall the technology is promising,” says Purna Kashyap, a gastroenterologist at the Mayo Clinic. If oxygen levels are proven to be a reliable proxy for location of the gas capsule within the gastrointestinal tract, the sensor, he says, “has the potential for significant impact in the future.”
But, Kashyap notes, ultrasound offers a relatively crude measure of intestinal movement. What’s more, the researchers only used the technology to benchmark the localization strategy in one individual. As such, he argues that it’s “premature to say this would be superior to breath testing”—the current standard for non-invasive gas analysis, which offers no positional information whatsoever—and he calls for “much more extensive validation.”
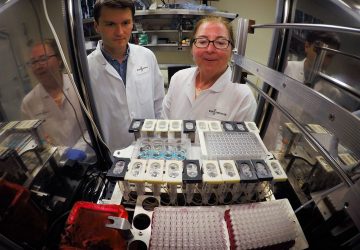
That validation is already underway. Last year, with grant support from the Australian government, Kalantar-zadeh and his clinical colleagues tested the capsule in 20 more healthy individuals. And although the results remain unpublished, according to Kyle Berean, a research fellow in Kalantar-zadeh’s lab: “The outcomes of our capsule were significantly better than those of the breath test.”
Berean says the team plans to further validate the positional accuracy of oxygen testing by using radiolabeled capsules and PET imaging. And they hope to run a much larger trial involving patients with gut disorders to see whether the capsule can accurately discriminate between small intestinal bacterial overgrowth, in which microbes that normally live in the colon have migrated upstream, causing problems, and other conditions.
First, however, they need to raise money—and the vehicle for that is their newly formed startup, Atmo Biosciences.
Last September, Atmo was one of six companies chosen for the inaugural cohort of ANDHealth, a new Australian accelerator program for digital health technologies that provides expert advice in starting a business in the medtech space and seed funding for consulting services. Among the 55 applicants for the program, Atmo stood out for having a “first-in-class technology with a massive unmet market need,” says ANDHealth managing director Bronwyn Le Grice.
“It’s got some very promising early data,” Le Grice adds. “Yes, they will need to raise capital, and, yes, they will need to launch further trials. But this has a really good chance of success.”
source: www.spectrum.ieee.org